
15
2.4
What works and what does not: Critical success factors and main risks in
improving the access to health services
Discussion on what works to improve access to quality healthcare, and what does not, is probably one
of the most challenging issues in current agendas. With the advent of health system research, there has
been remarkable improvement in the study of health disparity and how innovation can drive positive
changes. However, decades of experience in improving access to healthcare can attest that there is no
‘simple recipe’ for ensuring equitable access to healthcare everywhere. A recently published book has
critically reviewed reform in 60 countries across the globe, covering all continents and regions. The
book presents 60 case studies on reforms in different countries, with a view on policy change involving
systems, economic, methodological, implementational and practice related interventions. The reforms
under study range from policy, care coverage and governance, to quality, standards, accreditation and
regulation, organization of care, safety, workforce and resources, technology and IT, and practical ways
for stakeholders’ collaborations and partnerships. Four common principles leading to success in those
60 countries (Braithwaite et al., 2017; Jeffrey et al., 2017) were identified:
1.
The ‘acorn-to-oak tree’ principle = a small-scale initiative can lead to system-wide reforms,
2.
The ‘data-to-information-to-intelligence’ principle = the role of IT and data are becoming more
critical for delivering efficient and appropriate care, but must be converted into useful
intelligence,
3.
The ‘many-hands’ principle = intensive interaction between stakeholders is key, and
4.
The ‘patient-as-the-pre-eminent-player’ principle = placing patients at the centre of reform
designs is critical for success).
These four principles are an excellent summary of the on-going wide range of efforts that are shaping
present-day health system innovations globally. For example, investing into small projects like pilots
or modest innovations have helped shaping the health system environment to achieve UHC in
countries like Iran
(Figure 8shows trend of improvement for maternal deaths; WHO 2017b), New
Zealand, Estonia, Ecuador and Fiji. Information has a special role in ensuring access to healthcare by
all. By using technology for collection, analysis and dissemination to turn information into intelligence,
countries like Chile, UAE, South Africa
(Figure 8 shows trend of improvement for under five deaths;
WHO 2019), Ireland, China and Italy has made considerable improvement in providing high quality
and safe healthcare (
Ibid.
).
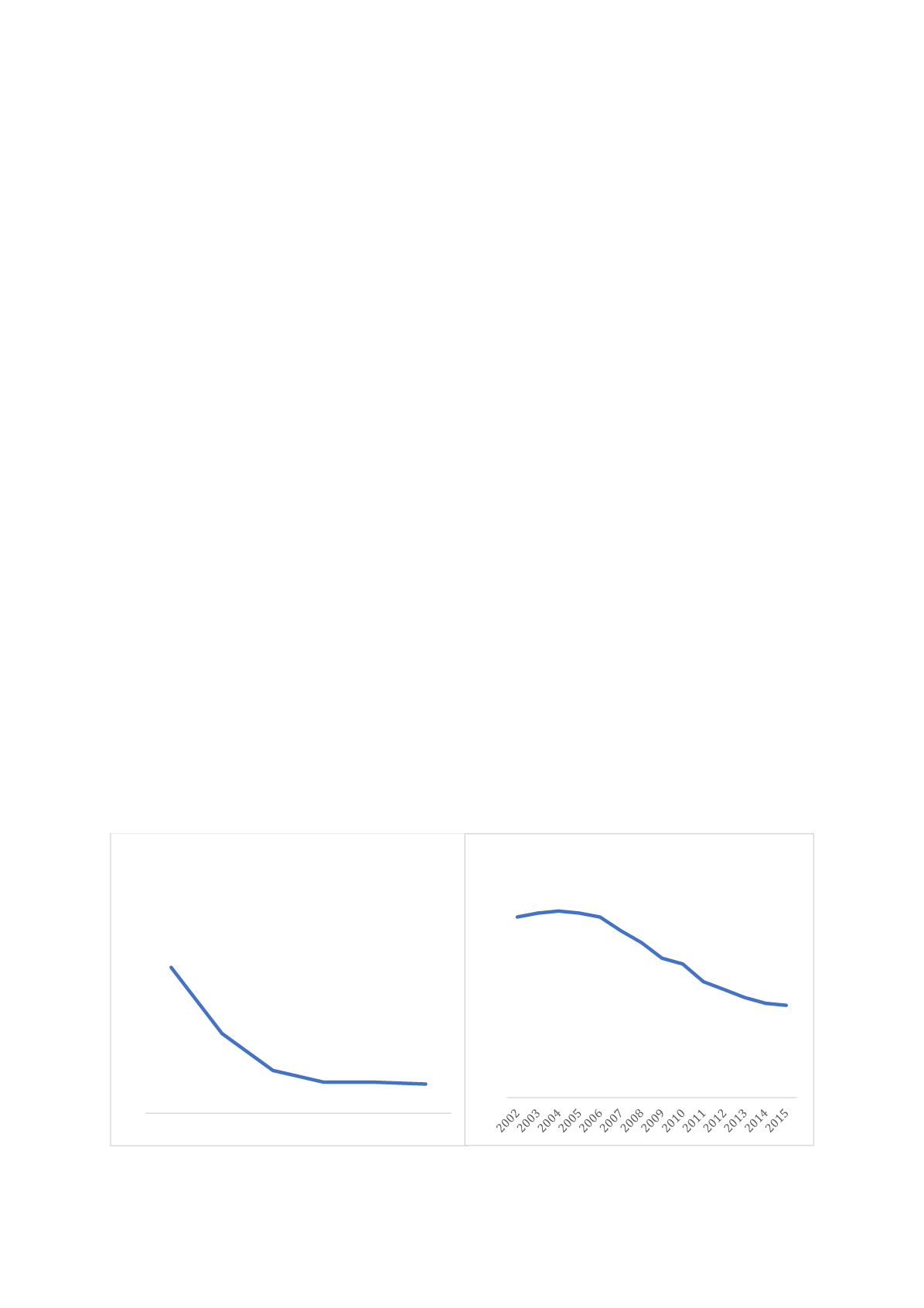
Figure 8: Proportion of maternal deaths among deaths of female reproductive age (PM %) in Islamic
Republic of Iran, (Left) and number of under-five death (in thousands) in South Africa, (Right)
Source: WHO 2017b and WHO 2019
7,5
4,1
2,2
1,6 1,6 1,5
0
1
2
3
4
5
6
7
8
9
10
1990 1995 2000 2005 2010 2015
Proportion of maternal deaths among
deaths of female reproductive age (PM
%), Islamic Republic of Iran
92 94 95 94 92
85
79
71 68
59
55
51 48 47
0
10
20
30
40
50
60
70
80
90
100
Number of under five death
(thousands), South Africa)
















