
32
and vaccines for all. For this, access to health will be conceptualized as four dimensions: (1) physical
accessibility (good services are within reasonable reach of everybody), (2) financial affordability
(people’s ability to pay without financial hardship), (3) acceptability (people’s willingness to seek
services and or utilization of condolences) and (4) people’s right to seek, receive and contribute health
related information.
3.4.
Access to healthcare services in OIC countries
Physical access to healthcare
Physical accessibility to healthcare crucially depends on the types and distribution of services and
related coverage by population and the location (rural/urban). Specific services in relation to maternal
and child health, family planning and communicable and non-communicable diseases which focuses
on increasing/improving access as well as better population targeting are of relevance here. How these
interventions/programs accessed by the people from low income groups in the OIC is an important
dimension of physical access. In what follows, we engage with a few of these indicators to examine the
physical dimension of healthcare access in OIC countries.
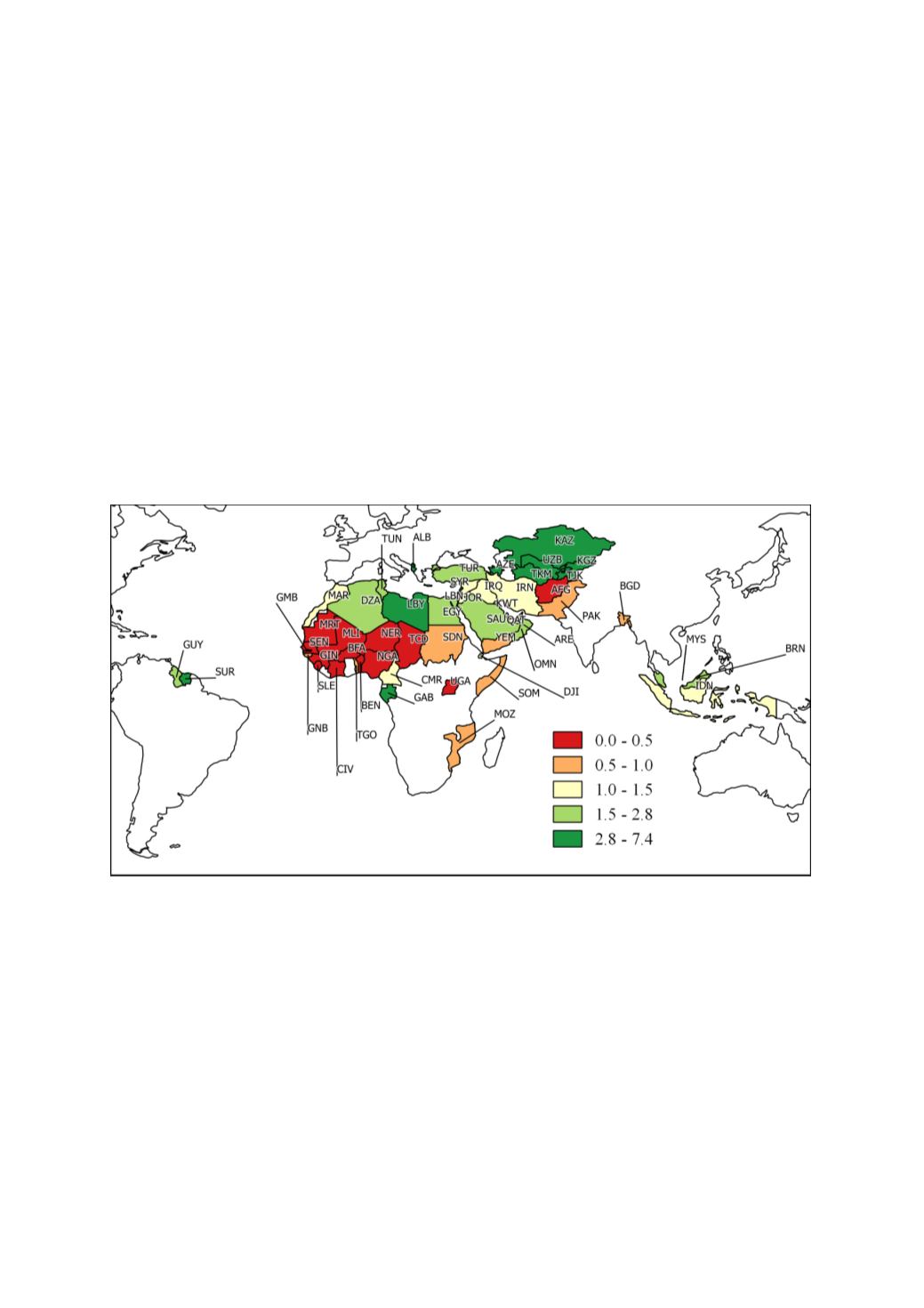
Figure 17: Hospital beds (per 1,000 people)
Figure 17maps the physical availability of hospital beds per 1000 people in OIC countries. Here the
hospital beds include inpatient beds available in public, private, general, and specialized hospitals and
rehabilitation centers. Availability and use of health services, such as hospital beds per 1,000 people,
reflect both demand and supply-side factors. Here we use it as a proxy indicator of the extent of
physical, barriers to health care. Figure 8 maps most recent hospital bed data for OIC countries (the
most recent data is dated 2015). The high level of variation in hospital beds among the OIC countries
is brought out by the large gap that exist between Kazakhstan (KAZ) with 6.7 beds in 2013 and Mali
(MLI) with 0.1 beds in 2010. Geographic clusters or country groups which share similar levels of
hospital bed provisions is also visible with very poor provisions in Sub-Saharan Africa and higher
levels seen in a cluster of central Asian OIC countries.
















