
5
Goals (MDGs), the health targets and indicators of SDGs 3 includes burden of disease; mortality and
morbidity. In addition, it also includes access to health services by including targets to trace level of
coverage of services, associated financial burden and broader system related indicators to address the
complex nature of health system.
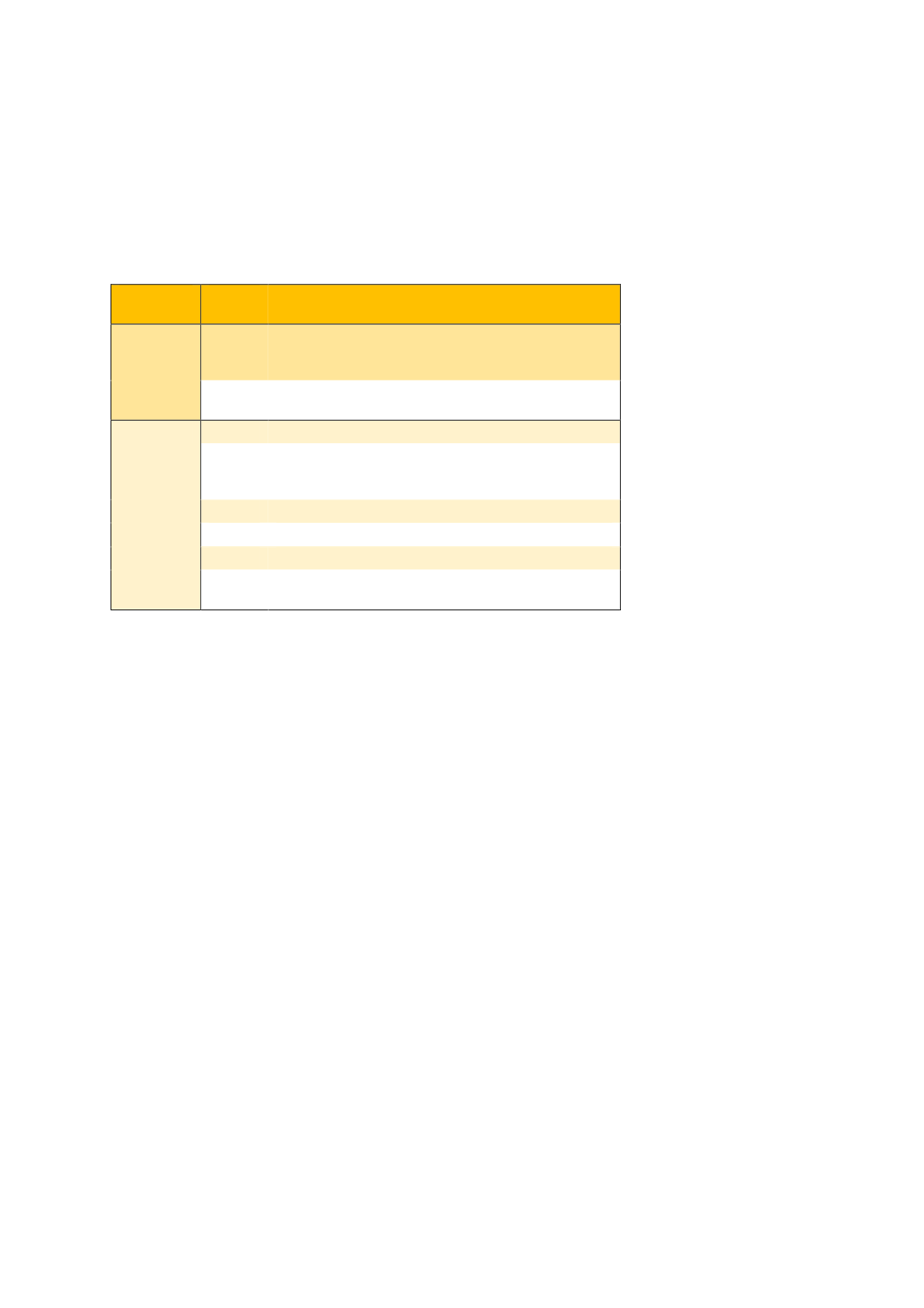
Table 1: Selected SDG targets and proposed indicators linked to health systems, by type of indicator
Type
of
indicator
SDG
target
Proposed indicator
Coverage/
financial
protection
3.8
UHC index: tracer indicators on service access (hospital
access, health workforce density by specific cadres,
access to medicines and vaccines, IHR capacities)
3.8
UHC:
financial
protection
(catastrophic
and
impoverishing out-of-pocket health spending)
System
3.b
Access to medicines and vaccines
3.b
Research and development on health issues that
primarily affect developing countries, including official
development assistance (ODA)
3.c
Health workforce density and distribution
3.d
IHR capacity and health emergency preparedness
17.18
Data disaggregation
17.19
Coverage of birth and death registration, completion of
regular population census
Table 1 shows the indicators that have been considered for health in SDG (Marmot and Bell 2018, WHO
2017, CIH 2018, WHO 2018). These indicators, target and goals are altogether inspired by universal
health coverage (UHC), a movement which started before the endorsement of SDGs to address the
growing health inequity in the world. UHC means that everyone has access to quality health services
without any financial hardship. It includes needed essential and quality health services; promotive,
preventive, treatment, rehabilitative and palliative care (WHO 2018b). While this is essentially a
responsibility of the national health systems, the complex nature of health system organization,
interaction between actors and lack of state’s stewardship and pro-people policy result into restricted
access to health services. The growing literature explaining the state of health equity and endorsement
of UHC through SDG is a global recognition that access to health services is a major challenge to achieve
sustainable development and well-being of the people.
Consequences of poor access to health services for the poor
Access to health services is particularly challenging for the poor. The disparity in organization of health
system and associated service provision directly affects the poor. Indicators in box 1 includes the
distribution of human resource for health (HRH). Evidence from Bangladesh shows there are
approximately five physicians and two nurses per 10,000 Bangladeshi. According to the World Health
Organization (WHO), the critical threshold for trained HRH is 23 (Ahmed et al. 2011,WHO 2014).
Among the qualified health personnel, there are twice as many doctors as nurses and doctors are
mostly clustered in urban areas. This shortage of trained state healthcare professionals and abundance
of private and informal healthcare provision has led Bangladesh to; a) restricted access to quality
healthcare (Iqbal et al. 2009) and b) increased healthcare expenditure. In 2012, the out of pocket (OOP)
expenditure for health was 64% of total healthcare expenditure (THE) ($4.1 billion), which was 93%
of total private expenditure (the figures for India and Nepal are 89.2% and Nepal 79.9%, respectively
(Adams et al. 2003, BHW 2012, HEU 2012, Molla and Chi 2017, Ahmed et al. 2015)). This is just one
example showing how inequitable and unjustified distribution of health system indicators can interact
















